What are Vein Valves?
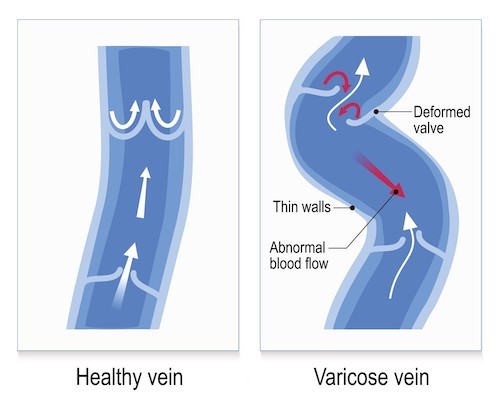
Interspersed throughout your veins are small crescent-shaped flaps of tissue, known as valves, that help prevent a backflow of blood. These valves project from the innermost layer of the vein wall to the center of the vein and are angled towards the heart in the direction of venous blood flow. Lacking muscles to open and close them, they work passively, like swinging doors. As blood flows past a valve it pushes the valve open and as the blood flow slows the valve swings back to its closed position.
What Causes Vein Valves to Become Damaged?
There are numerous causes for damaged vein valves, including:
The Aging Process
With age, the vein walls weaken and expand and the valve flaps may no longer reach each other in the closed position. This allows leakage or regurgitation of blood.
Weak Valves
Vein valves are made of a protein called collagen. The characteristics of collagen vary slightly from person to person, with some people producing more flexible collagen while others produce a version that is relatively stiffer. If you are in the latter group your valves may be more susceptible to wear and tear and more easily damaged.
Lack of Physical Activity
Muscular activity is important for healthy veins. As you contract your leg muscles, they gently compress the veins and assist the movement of blood through them. Having a desk or standing job that requires you to be sedentary for hours at a time reduces the beneficial effects of muscle activity and, as a result, blood flow becomes sluggish. Over time, this leads to venous hypertension causing the veins to expand and the valves to become leaky.
Female Hormones
Female hormones have significant effects on vein valves. Progesterone softens the walls of the veins and the valve tissue. High levels of progesterone, as during pregnancy, can cause the veins to expand and the valves to become leaky. Too much progesterone can also make the valves overly flexible and fail to close properly.
Estrogen provides important anti-inflammatory effects that protect vein valves from damage. As venous insufficiency increases, the number of estrogen receptors in the veins has been found to also increase and this is true for men as well as women[2].
Blood Clots
Valve damage can occur from a blood clot that develops in the leg, impairing blood flow. As backpressure builds the valve eventually gives way and opens in the wrong direction, sustaining damage in the process. Additionally, if a blood clot forms on a valve it can cause scarring that prevents the valve from opening and closing properly.
Accidents, Injuries, or Illness
Less commonly, a past accident or injury to the legs, surgery involving the legs, or a disease process that affects the circulation can also damage vein valves.
How Do I know If My Vein Valves Are Damaged?
As the number of damaged valves increases, the circulation in your legs will be significantly impaired. This condition, generally referred to as venous insufficiency, provides many symptoms that will undoubtedly get your attention.
Symptoms of venous insufficiency range from mild to severe and may include:
- Itchy, burning sensations in the legs
- Bulging veins
- Aching
- Heaviness
- Muscle fatigue
- Pain when walking that alleviates when you rest
- Leg cramps or muscle spasms
- Swelling in the legs or ankles
- Restless legs, especially at night
- Leg ulcers
- Dark, bruise-like discoloration of the skin around the ankles.
How are Damaged Vein Valves and Venous Insufficiency Treated?
A few simple self-care techniques can help you manage mild to moderate damaged veins and venous insufficiency symptoms.
One useful option is compression stockings, which help prevent blood from pooling and can reduce swelling and achiness. These are available over-the-counter or by prescription if you need higher levels of compression.

Exercise is your veins’ best friend and one of the best forms of exercise you can do for your vein valves is walking. Often touted as the ‘perfect’ exercise, walking lives up to its reputation for people with problem vein valves because it gets the muscular pump working in your legs and can reduce blood pooling and feelings of heaviness. Or, if you prefer a different activity you can choose swimming, dancing, or another form of exercise that gets your legs moving.
In-between exercise sessions get an assist from gravity by elevating your legs. Aim for two 30-minute sessions per day with your legs elevated above the level of your heart.
If your symptoms are more advanced or you are simply ready to ditch the compression stockings and opt for a more permanent solution there are several minimally invasive procedures that are performed in-office with only local anesthesia needed.
VenaSeal™is a permanent solution for varicose veins that works by injection of a medical-grade adhesive that closes off the affected veins and the blood is then rerouted to healthy veins
ClosureFast™ uses patented radiofrequency ablation (microwaves) to deliver uniform heat to treat and close affected veins and the blood is then rerouted to healthy veins.
Sclerotherapy is a treatment for spider veins where an injection of a liquid compound is introduced directly into the veins that cause the veins to become absorbed by the body and the blood is then rerouted to healthy veins.
To learn more about vein valves and these treatments, we invite you to schedule a free consultation at Empire Vein and Vascular Specialists. All of our physicians are board-certified vascular surgeons who specialize in helping people like you. Empire Vein and Vascular Specialists is the top provider of VenaSeal™, the leading outpatient varicose vein treatment, in the USA.
To schedule a free consultation, please call 1-888-263-7089 today.
Sources:
- Comparative study of the distribution of venous valves in the lower extremities of black Africans and Caucasians: pathogenetic correlates of prevalence of primary varicose veins in the two races. Anat Rec, 1987. 217(4): p. 407-12
https://pubmed.ncbi.nlm.nih.gov/3592268/ - Estrogen Receptors and Chronic Venous Disease. Eur J Vasc Endovasc Surg, 2016. 52(1): p. 114-8
https://pubmed.ncbi.nlm.nih.gov/27220899/